Fibroid Uterus

Uterine fibroids are also known as Myoma or Leiomyoma and are benign (non-cancerous) growths in the uterus. Fibroids develop from the cells that make up the muscle of the uterus. The size, shape, and location of fibroids can vary greatly and so do symptoms. Fibroids can range in size from small, pea-sized growths to large, round growths that may be like watermelon. A woman can have only one fibroid or can have happened many in number. Fibroids are generally slow-growing but sometimes they can grow rapidly. Many women who have fibroids are not even aware of them because the growths can remain small and not cause symptoms or problems. These often do not require treatment, but when symptomatic treatment may be advised.
How common are fibroids?
Fibroids are commonly seen in reproductive age group ranging 16 to 50 years of age when oestrogen hormone levels are at their highest. It is estimated that between two to four in every ten women have, or will develop fibroids at some point in their lives.

Research has shown that as many as one in five women suffer with heavy (menorrhagia) and painful periods (dysmenorrhoea). Every month, this can have a huge impact on your day-to-day activities, and cause social, emotional and physical distress. Your quality of life can be low during these days.
Heavy and painful bleeding can be a sign of a range of conditions, so instead of just attributing it to fibroid it is best to seek doctors help.
What are the causes of Uterine Fibroids?
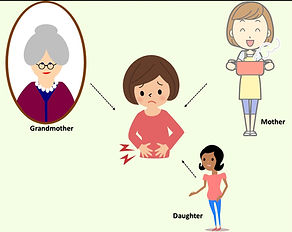
The exact cause as to why some women develop fibroid is still unknown. Studies have shown that there could be genetic component for development of fibroids.
Who is at risk of developing uterine fibroids?
Though we do not know the exact cause as to why women develop fibroid uterus, but there are various factors identified that can increase the risk of developing fibroids such as:
-
Age: Fibroids are commonly seen in reproductive age and they develop more common as women age, especially during their 30s and 40s and goes up to menopause. After menopause due to decrease in the hormones it has been noted that fibroids are much less likely to form and usually shrink if they’re present.

-
Obesity: Women who are overweight or obese may be at a higher risk of fibroids, as being overweight increases the amount of oestrogen in the body as the fat gets converted to oestrogen hormone through a peripheral fat conversion mechanism. It has been noted that for very heavy women, the risk is two to three times greater than average.

-
Ethnic origin: Fibroids are also found to develop more commonly in African-Caribbean populations than other ethnicities, although exact reasons for this are not clearly understood by scientists.

-
Family history: studies have shown there is some genetic link for development of fibroid, hence having a family member with fibroids increases your risk. If a your mom had fibroids, your risk of having them is about three times higher than average.
What are the types of fibroids?
Depending from which part of the uterus the fibroids develop there are different names given such as:
a. Subserosal fibroids: these fibroids develop on the outer wall of the uterus and usually cause no symptoms. However, if these grow big in size, they can put pressure on surrounding organs such as the bladder and the bowel.
b. Intramural fibroids: in this type fibroids develop within the wall (muscular layer) of the uterus. This is the most common type of fibroid that may cause symptoms.
c. Submucosal fibroids: in this type fibroids develop from the inner lining of the uterus. This is another common type to cause symptoms.
d & e. Pedunculate submucosal fibroid: in this type a submucosal fibroid will develop a long stalk and can sometime protrude through the cervix.
f. Broad ligament fibroid: in this type the fibroid develops from the outer surface of the uterus and buries itself in-between the lining of tissue situated next to the uterus called broad ligament. This general doesn’t cause any symptoms unless they grow large in size and puts pressure on surrounding organs.

What are the symptoms of Uterine Fibroids?

Changes in menstruation: heavy bleeding, long and painful period. Bleeding/spotting between periods. Sometimes there can be spotting per-vagina after sexual intercourse.

Pain: when fibroids are big they can cause heavy and aching in the abdomen and lower back. Sometimes when fibroids are big and occupying the whole pelvis there can be pain or discomfort during sex.

Pressure: sometimes big fibroids can press on to the bladder and cause frequent or difficult urination.

Constipation or difficult bowel movements: when fibroids are big they can press on to the rectum and cause bowel symptoms.

Bloated abdomen: when the fibroid grows you may notice that your belly is becoming big just like pregnancy.

Pregnancy complications: fibroids tend to grow during pregnancy and can cause miscarriage, abortions, abnormal lies of the fetus in the womb. During pregnancy, fibroids undergo red degeneration and can cause severe pain.

Infertility: sometimes fibroid can cause infertility.

Anemia: due to chronic heavy menstruation your hemoglobin levels can decrease leading to symptoms such as tiredness, dizziness, weakness, and headaches.
What tests will be required for diagnosis?
-
Physical examination: If you have symptoms of fibroid you may be advised to undergo physical examination like palpating your abdomen and internal examination to know the size of the uterus. As the uterus is generally larger than normal, a pelvic or internal examination may determine that the womb is enlarged. This may be the first investigation that suggests you have fibroids.
-
Ultrasound: A pelvic ultrasound performed vaginally (internal) or abdominally (tummy) will not only diagnose fibroids in the womb but it also shows the number and positions of fibroids in the uterus.
-
MRI (magnetic resonance imaging) scan: Occasionally a more detailed scan called MRI may need to be performed to diagnose the fibroid uterus more accurately.
-
Hysteroscopy procedure: Sub-mucous fibroids which occur on the inside of the womb can be diagnosed by a hysteroscopy procedure. This procedure involves passing a small telescope (hysteroscope) through the cervix (the neck of the womb) and into the uterus. Hysteroscopy can not only diagnose submucous fibroids but they can also be removed at the same time. This procedure is under anesthesia.

What are the treatment options for Uterine Fibroids?
-
Conservative management (observation): Fibroids that do not cause symptoms often do not require treatment. Most of the time fibroids are incidentally picked up during ultrasound, in such situations you don’t need any treatment.
Medical Management:
Medication for pain:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as mefenamic acid or ibuprofen, help reduce menstrual blood loss. NSAIDs also have the added benefit of relieving painful menstrual cramps (dysmenorrhea).
Medication to decrease bleeding:
-
Tranexamic acid: Tranexamic acid is an antifibrinolytics group of medications that help reduce menstrual blood loss and only needs to be taken at the time of the bleeding.
-
Oral contraceptive pills (OCP): apart from providing birth control, oral contraceptives can also help regulate menstrual cycles and reduce excessive or prolonged menstrual bleeding. This is generally taken for 21 days and repeated cyclically.
-
Oral progestogen: Oral progestogen given in form of can help reduce heavy periods. It's usually advised to be taken on a daily basis starting from days 5 to 26 of your menstrual cycle, counting the first day of your period as day 1. This works by making the womb lining grow slowly.
-
Injected progestogen: progestogen is also available as an injection to decrease heavy periods. It works similarly to oral progestogen.
-
Hormonal Intrauterine Device (IUD): Mirena this IUD releases a type of progestin called levonorgestrel into the uterus and makes the uterine lining thin and thus decreases menstrual blood flow and cramping. This device also acts as a contraceptive method like Copper-T.

Non-surgical procedure:
-
Uterine artery embolisation: as fibroids develop from the uterus they also share blood supply of the uterus, this is a procedure that involves blocking the main blood vessels to the fibroid in order to stop the growth of the fibroids. This procedure is exactly like cardiac stenting where in it involves a small cut in the groin area and a small tube is then passed through the blood vessel to reach main arteries that is feeding the fibroid and tiny particles are injected to cut off the blood flow. Post procedure, many women experience cramping for a few hours after the procedure. Some women complain of nausea or fever. There is a small risk of developing severe infection and hysterectomy may be required. The effects of uterine artery embolisation on a woman's fertility is not known. Women who wish to have children may want to consider all other options of fertility preservation.

-
HIFU: High-intensity focused ultrasound (HIFU) this is a non-surgical (non-invasive) treatment for fibroid uterus that uses non-ionizing ultrasonic waves to focus at point and heat tissue and destroy the tissue following which the body absorbs the dead tissue. Treatment for symptomatic uterine fibroids became the first approved application of HIFU by the FDA (US Food and Drug Administration) in October 2004. Various studies have shown that HIFU is safe and effective, and that patients have had symptomatic without the risk of complications involved in surgery or other more invasive approaches. It’s important to note that up to 16-20% of patients will require additional treatment.


Surgical Management
In some situation when medical management fails or when fibroid is of big size causing pressure symptoms then you would be advised surgery such as:
-
Myomectomy: myomectomy is an operation that involves removing the fibroids from the uterus and retaining the uterus. This option is given when the lady is symptomatic and wants to retain her uterus to become pregnant. Myomectomy operation can be done via hysteroscopy, laparoscopy, robotic or laparotomy depending on the size and the location of the fibroids. It’s important to remember that sometimes after myomectomy there could be internal scarring in the lining of the uterus and that can lead to infertility. During myomectomy procedure if the uterine cavity (endometrium) is entered then your doctor would advise you to be cautious during your pregnancy as in some rare situation it can lead to uterine rupture and also there is high chance that you may be advise to undergo elective caesarean section type of delivery of the baby. Note: fibroids may re-develop again, after the surgery and further surgery is usually required in 20 to 40 per cent of cases.

-
Hysterectomy – in some situation when family is complete hysterectomy would be is an operation to remove the uterus with the fibroids and the cervix as well.
Can fibroids during pregnancy cause any complications?
When women who have fibroids conceive they are more likely to have problems during pregnancy and delivery. Most of the women with fibroids have normal pregnancies. The most common problems seen in women with fibroids during pregnancy and delivery are:
-
High risk for caesarean-section, it has been noted that the risk of needing a C-section is six times greater for women with fibroids.
-
Baby can go into breech presentation and which is NOT normal position for normal vaginal delivery. For normal and uncomplicated delivery, babies head has to be down (cephalic presentation).
-
Sometime labor fails to progress.
-
Can rarely lead to placental abruption - here the placenta breaks away from the wall of the uterus before delivery (normally the placenta has to separate after delivery of the baby). When this happens, the bay does not get enough oxygen and can lead to fetal distress.
-
Sometimes it can cause preterm delivery.

Fetus
Fibroid
Can Uterine fibroids turn into cancer?
Fibroids are almost always non-cancerous (benign) and studies have shown that less than one in 1,000 a cancerous fibroid can occur. The cancerous counterpart is known as leiomyosarcoma. Studies are yet to prove that an already-existing fibroid can turn into cancer. If you have a fibroid it does not increase the risk of it developing into a cancerous fibroid. Having fibroids also does not increase a woman's chances of getting other forms of cancer in the uterus such as endometrial cancer.
